 ASPIRE Nursing Process ASPIRE Nursing Process What is a Nursing Care Plan? Nursing care plans are tools utilised by Registered Nurses to identify the existing needs of patients as well as potential needs or risks that may arise during a patients journey. Care plans enable nurses to make justified and rational decisions to improve patient care. They also provide a platform for communication between nurses and other members of the interdisciplinary team such as medical officers, physiotherapists, social workers, etc. Without care plans, quality and consistency of patient care would be lost. All hospitals and facilities differ in the format and style of nursing care plans that they use, some use standardised care plans and pathways and others allow greater scope for nursing staff to make independent decisions for their patients. Ideally, care plans should allow for a degree of independent nursing scope as holistic, patient centred and individualised care is considered best practice. Regardless of the type of care plan, this post will focus on the rationale behind care plans rather than the actual care plan itself. The objectives of a care plan -
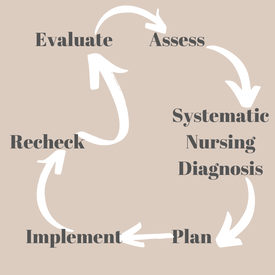
APIE vs ASPIRE? For most nurses, we will be familiar with the APIE (Assessment, Plan, Implementation & Evaluation) which is taught broadly across nursing schools in recent times. APIE was introduced in 1967 by Yura & Walsh and was referred to as 'the Nursing Process'. The aim of APIE was to move away from providing care 'because that is how we have always done it', to a more holistic and systematic approach. The APIE framework provides a basic guide to assist nurses in the formulation of a care plan, however the ASPIRE approach fills in the missing steps of the problem-solving approach. The steps of Aspire are Assess, Systematic Nursing Diagnosis, Plan, Implement, Recheck and Evaluate. These six stages are part of a cyclical pattern that is used to guide our nursing care. 1. Assess A large proportion of nursing care is around admission and assessment (and yes, they are very different things. One can do an admission without much thought to an assessment of the patient!). Admission relates to introducing yourself to the patient and making the patient familiar with the healthcare facility, and of course completing the required documentation. Assessment relates to a full physical, psychological, social, and cultural assessment. See here for my guide to a physical assessment. In regards to formulating a care plan, this part of the cycle should also include an assessment on the potential risks and needs that may arise. The assessment should be an objective, accurate and detailed account of the patient and their life. Some questions that might be valuable to complete an accurate assessment for a care plan include; what is the patient normally like?, what is the patient like now?, what is the change?, what has caused the change?, what can the patient do about the it?, what can we do about it?, does the patient have the necessary resources to cope? The next stage of the process will become substantially easier if a comprehensive patient assessment is undertaken. 2. Systematic Nursing Diagnosis The four stage APIE process does not include a nursing diagnosis stage, however nursing diagnosis is paramount to care planning. As registered nurses, we can diagnose our patients using nursing diagnostic frameworks. Most commonly we use the NANDA-I to guide our diagnosis. Nursing diagnosis emphasises the holistic needs of the patient. An effective assessment allows for easy identification of nursing diagnosis's. (For a list of NANDA-I approved diagnosis please click this link). It is important to remember that nursing diagnosis is different from medical diagnosis. For example, a nursing diagnosis would be 'ineffective airway clearance' whereas the medical diagnosis is 'pneumonia'. Commonly, nursing diagnosis relate to medical diagnosis and they go hand-in-hand. Once nursing diagnosis are established (and remember to document them), we can begin to plan interventions that may be of benefit for the patient. 3. Plan This stage of the ASPIRE framework involves thinking of interventions for the patient, and writing the actual care plan. The care plan will be utilised by all members of the nursing and interdisciplinary team, so it is important to make it thorough, evidence based, and easy to follow. The interventions in the care plan should achieve two goals; firstly, being individualised to respect the holistic needs of the patient, and secondly, be grounded in evidence based nursing to provide a rationale for the care we are prescribing and providing. The first goal is achieved by incorporating the patient as an integral part of the care. Without the patient, we would not be here. Gather information from the patient about their goals and expectations of the health service, and what they want to achieve in terms of their care. The second goal is achieved by using our nursing diagnoses (from step 2) to develop interventions which address these. The rationale for these interventions will be based upon the diagnosis, and it is important for nurses to use up to date knowledge to guide these. The care plan and interventions also act as a contractual agreement between healthcare provider and patient. Respect for individuality must always be upheld when developing a plan of care. Using the above example, ineffective airway clearance, the following interventions can be made:
It is also just as important to implement interventions to prevent perceived risks or potential problems from becoming actual problems. 4. Implement This is the 'doing' part of the cycle. So, now that we have a care plan and interventions for our patient, how do we go about completing them? This stage of the ASPIRE framework may seem ambiguous, and thats because it is. Each patient is an individual, therefore there is no correct or incorrect way to undertake interventions. It would also be impossible to write about all the ways nurses can implement care and interventions. As long as the interventions are grounded in evidence, within your scope and individualised to respect the needs and dignity of the patient, then they are correct. Remembering always that our interventions should not cause harm (non-maleficence). When providing care for our patients it is paramount that we respect their wishes, maintain their dignity, and empower them to become agents in their own healthcare. Cultural and individual differences between patients will greatly influence the way we care for our patients. Additionally, the status of our patient will greatly impact the way we give care. For example, providing hygiene care for an ambulatory patient on a ward is greatly different to providing hygiene for an ICU patient. Many considerations play an integral part of implementing care, these are; is the care individualised and patient centred? Is the care safe, legal and ethical? Is the care within my scope?, Is the care evidence based?, Do I need to gather consent prior to providing this care?, Did I uphold respect and dignity for my patient?, Do my interventions relate to my nursing diagnosis?, Did I communicate with the patient, their family and/or their carer?, and did I document my actions? 5. Recheck As part of this process, rechecking ensures that our interventions are meeting their goals. This is something that the APIE framework does not include, but is important to ensure that we providing the best care possible. Rechecking is a formative process whereby the nurse works with the patient to understand whether or not the interventions and care plan are working. The patient is central to this process, do they believe that they are getting better? It is also important for the nurse to continuously undertake assessment and monitor the patients progress. This data, as well as the patient views allow the nurse to understand what parts of the care plan are working well, and which parts of the care plan need to be readdressed. When parts of the care plan are working well, the nurse can leave these as is. However, if areas of the care plan need to readdressed and modified the nurse should being at step 1 again, and work their way through. This is the cyclic part of the framework which means that as nurses we are always striving to provide better care and better our patient outcomes. This stage also highlights patient deterioration. As we perform a reassessment of the patient any changes or differences can be noted and addressed. Remember to also document your recheck of the patient as it is important to note which interventions work well, and which do not. 6. Evaluate Recheck and evaluation are very similar in the fact that they both reassess to see if the patient has improved or deteriorated. However, recheck often looks specifically at the effectiveness of each interventions and allows for adjustments in the care plan. Evaluation examines the patients goals more broadly, and whether the experience was right for them as an individual. Evaluation is a cumulative tasks that requires the nurse to think about each step in this framework (baseline, goals, and recheck), and more broadly to think about each step of the patient journey. By doing this, nurses are evaluating the process and the outcome. This process allows the nurse to make changes to the process and improve themselves the next time they make a care plan for a patient. If you found this interesting, I highly recommend the book 'Care Planning - A guide for nurses' 2nd edition (2012) by Barrett, Wilson and Wollands.
0 Comments
Leave a Reply. |
|